Current status of ABL tyrosine kinase inhibitors stop studies for chronic myeloid leukemia
Introduction
ABL tyrosine kinase inhibitor (TKI) imatinib mesylate dramatically improves chronic myeloid leukemia (CML) prognosis. It has also become possible to utilize second-generation ABL TKIs that were developed to overcome imatinib resistance and intolerance. Most CML patients can now expect long-term survival. As a result of the introduction of ABL TKIs, most CML patients are now able to lead lives that are equivalent to those of healthy individuals (1).
However, in spite of improvements in prognosis, high cost to CML patients of long-term treatment and adverse effects (AEs) remain problems. Since CML is no longer a fatal disease in most cases, it is estimated that in the US the number of CML patients will rise 9-fold to 180,000 in 2050 as compared to the year 2000 (2). Long-term ABL TKI use entails not only the problem of individual cost burden but also the problem of increased overall medical costs.
In actual clinical settings, even if imatinib was discontinued for some reasons, occasionally there had been cases in which relapse were not observed over the long term. Thus, a clinical study involving the discontinuation of imatinib was first conducted in France (3). The results indicated that although it was not yet known of cure was achieved, in approximately 40% of patients who maintained complete molecular response (CMR) for at least 2 years due to imatinib, discontinuation of imatinib was possible over the long term (4). Subsequently, imatinib stop studies have been actively conducted around the world, including in Japan. In addition, several stop studies of second-generation ABL TKIs (dasatinib, nilotinib), which induce earlier response than imatinib, have also been started. Our group has already reported an interim analysis on dasatinib discontinuation study (5).
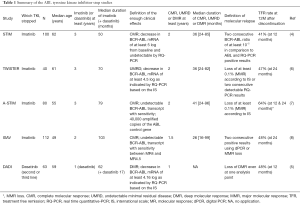
In this review article, I summarize the ABL TKI stop studies that have already been conducted (Table 1).
Full table
Clinical studies of imatinib discontinuation
Stop imatinib (STIM) study
STIM study in which imatinib administration to patients who had been taking imatinib and in whom BCR-ABL mRNA was not detected for at least 2 years using real-time quantitative PCR (RQ-PCR) was discontinued was conducted in France. Molecular relapse was defined as two consecutive RQ-PCR positive results. In 2010 the results of mid-term analysis indicated that 100 cases maintained CMR for at least 2 years as a result of at least 3 years of imatinib administration (4). The definition of CMR in the STIM study was a decrease in BCR-ABL mRNA of at least 5 log from baseline and undetectable by RQ-PCR. Molecular relapse was defined as two consecutive BCR-ABL ratio of at least 10−5 in comparison to ABL and RQ-PCR positive results. Forty-three percent of patients 12 months after discontinuation of imatinib and 41% of patients 24 months after discontinuation of imatinib maintained CMR and did not experience molecular relapse. Fifty-eight of the 61 cases that experienced molecular relapse, relapsed molecularly within 7 months after discontinuation of imatinib. All patients who experienced molecular relapse kept sensitivity to imatinib after resumption of imatinib administration. These results suggest that, based on careful observation, imatinib discontinuation is relatively safe (4).
Japanese retrospective study
In Japan, a retrospective study of imatinib discontinuation was conducted on 43 cases (9). It found that 47% maintained treatment-free remission (TFR; previously described as “cure” or “functional cure”, but currently generally mentioned as TFR).
TWISTER study
The Australasian Leukaemia & Lymphoma Group conducted a TWISTER study on 40 cases of chronic phase CML (6). Due to the difficulty of standardizing quantitative tests of BCR-ABL mRNA and the fact that the definition is unclear, in this study the term “CMR” was not used. Instead, based on the international scale (IS), “undetectable minimal residual disease” (UMRD) was defined as a decrease in BCR-ABL mRNA of at least 4.5 log (0.0032% or below) as indicated by RQ-PCR [currently “deep molecular response” (DMR) is widely used instead of either CMR or UMRD]. Forty patients who maintained UMRD for at least 2 years were selected as the subjects for discontinuation from a group that underwent imatinib therapy for at least 3 years. In this study, “molecular relapse” was defined as the loss of at least 0.1% major molecular response (MMR) according to IS or 2 consecutive detectable RQ-PCR results (UMRD loss). The TRF rate after 2 years of discontinuation was 47.1%. As with the STIM study, all patients in this study who experienced molecular relapse regained UMRD once imatinib therapy was resumed.
BCR-ABL mRNA level does not necessarily correspond to the number of residual CML cells. TWISTER study investigated not only mRNA but also residual patient-specific BCR-ABL DNA. Even though TFR was maintained (=BCR-ABL mRNA was undetectable), BCR-ABL DNA was detectable in most patients several years after imatinib discontinuation. This indicates that it is extremely important to consider the significance of TFR and relapse (10).
According to stop imatinib (A-STIM) study
The group that conducted STIM study also conducted A-STIM study in which they investigated a new ABL TKI discontinuation criterion (7). A-STIM study defined molecular relapse not as DMR loss (nearly the same definition as CMR and UMRD) but rather as MMR (0.1% or under according to IS) loss. At 24 months after discontinuation, 64% of the patients had not lost MMR and did not resume imatinib administration. After imatinib discontinuation 31% of the patients had levels under MMR, showing that there was variation in mRNA levels. This suggests that when ABL TKIs are discontinued after maintaining DMR for a sufficient period of time, MMR loss may be a practical and safe criterion for resumption of ABL TKI therapy. If it were possible to delay resumption of ABL TKI therapy until MMR loss, more patients would be able to spend longer periods of time without ABL TKI administration.
Imatinib suspension and validation (ISAV) study
ISAV study was conducted in order to investigate whether digital PCR (dPCR), which was more sensitive than conventional RQ-PCR and was able to detect single cell in 107BCR-ABL positive cells, was able to increase the success rate of imatinib discontinuation (8). One hundred twelve cases that were negative for at least 18 months according to dPCR after at least 2 years of imatinib administration were observed for 36 months. In this study molecular relapse was defined as either two consecutive positive results using dPCR or MMR loss. TRF was maintained in 51.9% of the cases. One hundred percent of patients aged under 45 who were dPCR positive experienced molecular relapse, but only 36% of patients aged 45 and over experienced molecular relapse. Although dPCR was effective in the ISAV study, because dPCR produces false positives, this issue requires further study.
EuroSKI study
A mid-term analysis was released at the 6-month point for 200 subjects who maintained DMR (in this study DMR was defined as MR 4.0; IS <0.01) for at least 1 year after having been administered either type of ABL TKI (imatinib 97%, second-generation ABL TKI 3%). The median administration period until ABL TKI discontinuation was 8 years (16% had a treatment history of at least 5 years). Molecular relapse was defined as MMR loss, and 61% of the subjects maintained TFR (11).
Results of stop studies of second-generation ABL TKIs
Even with 5 to 7 years of imatinib treatment, only approximately 40% of patients reach MR 4.5, which indicates a BCR-ABL mRNA decrease of at least 4.5 log—the definition of DMR in most stop studies (12). Nilotinib, dasatinib, and other second-generation ABL TKIs are more effective than imatinib and more patients achieve MR 4.5. In the ENESTnd study, 40% of patients who were administered 300 mg of nilotinib twice per day (BID) and 23% of patients who were administered 400 mg of imatinib once per day (QD) achieved MR 4.5 within 4 years (13). In addition, in a DASSISION study, 22% of patients who were administered 100 mg of dasatinib QD and 12% of patients who were administered 400 mg of imatinib QD achieved MR 4.5 by the 3-year mark (14). DMR achievement is the minimum requirement for TFR. Therefore, the use of second-generation ABL TKIs provides more CML patients with the right to attempt discontinuation. Thus, in addition to the STOP-2G-TKI study under way mainly in France, many stop studies of second-generation TKIs are currently being conducted both in Japan and abroad.
We conducted a clinical study of dasatinib discontinuation used in secondary or later treatment. This study was known as the Dasatinib Discontinue (DADI) Trial (principal investigator: Shinya Kimura) (5). Dasatinib treatment was discontinued for 63 CML patients who were switched to dasatinib for secondary treatment (some were switched for tertiary treatment) depending upon whether the patients were resistant to imatinib or not and maintained DMR for at least 1 year. Most previous STIM and other studies of ABL TKI discontinuation used at least 2 years of DMR maintenance as the condition for discontinuation, but the fact that the DADI trial used a shorter DMR period of at least 1 year was a characteristic of this study. The definition of DMR used in DADI trial was undetectability by RQ-PCR conducted at the central laboratory (equivalent to IS 0.0069%). After therapy discontinuation, loss of DMR even at one analysis point was defined as stringent molecular relapse, triggering therapy resumption. Forty-eight percent achieved TFR during the first year after dasatinib discontinuation. Fifty-two percent of the molecular relapse cases also re-achieved DMR within 6 months due to resumption of dasatinib administration. The results of DADI Trial suggest that dasatinib can be safely discontinued for approximately half of the patients who were treated with dasatinib for secondary or later treatment (5).
French group also reported the results of a stop study of 52 patients who maintained DMR for at least 2 years after administration second-generation ABL TKIs (either nilotinib or dasatinib). In this study, molecular relapse was defined as MMR loss. At the mean observation period of 32 months 54% had maintained TFR. The 12-month TFR rate was 42% for imatinib-resistant patients and 67% for imatinib non-resistant (non-intolerant) patients (15).
Safety of discontinuation
When discontinuation of ABL TKIs is attempted, the most concerning risk is the possibility that when molecular relapse occurs the ABL TKI will have lost the effectiveness it had prior to discontinuation, which would cause the patient’s condition to be exacerbated. Although at least 1,000 subjects who have discontinued ABL TKIs have been studied up to the present time in all but one case, ABL TKIs were successfully used after therapy was resumed. This patient was not typical of the contemporary CML population, and had started imatinib ten years after her original diagnosis of CML. She lost MMR after stopping imatinib, and was responsive to re-treatment, but 8.5 months later developed blast crisis (7). It is still controversial when we must re-administrate TKIs after molecular relapse. Tsutsumi et al. recently reported two cases that spontaneously achieved CMR and two cases that remained in CHR without TKI treatment with a median follow-up of 29.5 months. Thus, the survival of patients who lost CMR following TKI discontinuation may not be affected, even without re-administration of TKIs (16).
Recently, the issue of withdrawal syndrome after ABL TKI discontinuation has become a problem. There are also sporadic reports of approximately 15–30% of patients who suffered slight symptoms after discontinuation of ABL TKI, such as muscle pain, joint pain, bone pain, rash, depression, weight loss, and others (17,18). The cause of withdrawal syndrome is still controversial.
When attempting ABL TKI discontinuation, there are also psychological problems. A certain number of patients experience extreme fear of relapse caused by discontinuation of the drug, and it has been reported that approximately half are anxious that they will lose therapeutic response (19).
Predictive factors for successful discontinuation
Patient background characteristics
In the STIM study, male patients with low Sokal scores and a history of imatinib administration of at least 50 weeks had a significantly low rate of molecular relapse after imatinib discontinuation (4). In the TWISTER study and a retrospective study conducted in Japan, it was shown that a history of interferon (IFN)-α use contributed to higher TRF rates (6,9). In addition, cases with a short history of INF-α therapy and delayed achievement of UMRD after switching to imatinib had a significantly high risk of molecular relapse (6). In the ISAV study, patients with few remnant lesions had a higher TRF rate than those aged 45 and over (8). Also, DADI trial provided important suggestions regarding discontinuation of second-generation ABL TKIs used as a second line therapy. Sixty-one percent of cases that were switched to dasatinib due to imatinib intolerance achieved TFR in at least 1 year, but only 8% of patients who were switched to dasatinib due to imatinib tolerance achieved TFR after at least 1 year (5).
Based on these results, currently the following patients are not indicated for ABL TKI discontinuation: (I) those with intermediate or high Sokal scores; (II) those tolerant of ABL TKI prior to treatment; and (III) those with non-traditional bcr-abl transcriptional products (minor bcr-abl, etc.) that cannot be reliably monitored.
Immunological parameters
Since ABL TKIs are not effective on CML stem cells, many questions remain regarding why TFR can be achieved. It is assumed that immune cells suppress minimal residual disease, which then contributes to TFR maintenance.
Transplanting NK cells into irradiated mouse bone marrow has shown that NK cells play an important role in the onset of CML (20). Clinically, prior to the appearance of ABL TKIs, NK cell increases were reported in patients who discontinued IFN-α, the drug of first choice (21). In addition, CML patients who maintained DMR after discontinuation of imatinib had a higher ratio of functional NK cells than healthy individuals and patients who maintained MMR for at least 2 years due to imatinib in spite of losing DMR after discontinuation (22).
It is well-known that dasatinib causes increases in large granular lymphocytes (LGLs), and that it has a high degree of therapeutic effect in cases with increased LGLs (23,24). LGL is a morphological name that includes cytotoxic T cells (CTLs) and NK cells. In DADI trial, there was a decrease in regulatory T cells during the dasatinib administration period and cases in which NK cells increased had a significantly high TFR rate. However, increases in CTL did not contribute to TFR rate (5). Based on these results, currently it is thought that NK cell immunity is more important to the TFR of CML patients than CTL.
Future prospects
In cases in which the first attempt at ABL TKI discontinuation failed, are all chances lost? Although only a small number of cases were studied, it has been reported that 20% of patients who made a second attempt achieved TFR (25). In addition, in order to increase the TFR rate, we anticipate that it will be necessary to utilize combined administration of drugs (Wnt/β-catenin inhibitor, hedgehog inhibitor, etc.) that are thought to be effective on CML stem cells.
ABL TKI discontinuation in actual clinical practice
European LeukemiaNet recommends that currently “People who achieve optimal response should continue taking ABL TKIs, and discontinuation should only be done as part of clinical studies. Discontinuation may be considered in cases of women who hope to become pregnant and who maintained CMR for at least 2 years only after obtaining their informed consent.” (26). Ideally, all cases who participate in clinical studies should undergo ABL TKI discontinuation. In comparison to the many patients who desire discontinuation, there are few studies of discontinuation being conducted, which has resulted in a large number of “ABL TKI Stop refugees”. In a review published in the journal Blood, Hughes et al. expressed the opinion that “We acknowledge that there are potential risks associated with cessation attempts in wider clinical practice, but this should not deter us. Instead we need to establish criteria for safe and appropriate TKI cessation. Clinical trials will enable us to define the best strategies to achieve TFR, but clinicians need guidance today about how to approach this issue with their patients.” (27).
Conclusions
In the future, more and more ABL TKI stop trial results will be reported around the world. It is important to conduct a comprehensive examination of the results of studies with a wide variety of protocols (the definition of DMR and molecular relapse, etc.) in order to determine which discontinuation method results in the highest probability of TFR in clinical settings.
Acknowledgements
None.
Footnote
Conflicts of Interest: Shinya Kimura; Honoraria: Bristol-Myers Squibb, Pfizer, Research Funding: Bristol-Myers Squibb, Novartis.
References
- Sasaki K, Strom SS, O'Brien S, et al. Relative survival in patients with chronic-phase chronic myeloid leukaemia in the tyrosine-kinase inhibitor era: analysis of patient data from six prospective clinical trials. Lancet Haematol 2015;2:e186-93. [Crossref] [PubMed]
- Huang X, Cortes J, Kantarjian H. Estimations of the increasing prevalence and plateau prevalence of chronic myeloid leukemia in the era of tyrosine kinase inhibitor therapy. Cancer 2012;118:3123-7. [Crossref] [PubMed]
- Rousselot P, Huguet F, Rea D, et al. Imatinib mesylate discontinuation in patients with chronic myelogenous leukemia in complete molecular remission for more than 2 years. Blood 2007;109:58-60. [Crossref] [PubMed]
- Mahon FX, Réa D, Guilhot J, et al. Discontinuation of imatinib in patients with chronic myeloid leukaemia who have maintained complete molecular remission for at least 2 years: the prospective, multicentre Stop Imatinib (STIM) trial. Lancet Oncol 2010;11:1029-35. [Crossref] [PubMed]
- Imagawa J, Tanaka H, Okada M, et al. Discontinuation of dasatinib in patients with chronic myeloid leukaemia who have maintained deep molecular response for longer than 1 year (DADI trial): a multicentre phase 2 trial. Lancet Haematol 2015;2:e528-35. [Crossref] [PubMed]
- Ross DM, Branford S, Seymour JF, et al. Safety and efficacy of imatinib cessation for CML patients with stable undetectable minimal residual disease: results from the TWISTER study. Blood 2013;122:515-22. [Crossref] [PubMed]
- Rousselot P, Charbonnier A, Cony-Makhoul P, et al. Loss of major molecular response as a trigger for restarting tyrosine kinase inhibitor therapy in patients with chronic-phase chronic myelogenous leukemia who have stopped imatinib after durable undetectable disease. J Clin Oncol 2014;32:424-30. [Crossref] [PubMed]
- Mori S, Vagge E, le Coutre P, et al. Age and dPCR can predict relapse in CML patients who discontinued imatinib: the ISAV study. Am J Hematol 2015;90:910-4. [Crossref] [PubMed]
- Takahashi N, Kyo T, Maeda Y, et al. Discontinuation of imatinib in Japanese patients with chronic myeloid leukemia. Haematologica 2012;97:903-6. [Crossref] [PubMed]
- Ross DM, Branford S, Seymour JF, et al. Patients with chronic myeloid leukemia who maintain a complete molecular response after stopping imatinib treatment have evidence of persistent leukemia by DNA PCR. Leukemia 2010;24:1719-24. [Crossref] [PubMed]
- Mahon FX, Richter J, Guilhot J, et al. Interim analysis of a pan European stop tyrosine kinase inhibitor trial in chronic myeloid leukemia: the EURO-SKI study. Available online: https://ash.confex.com/ash/2014/webprogram/Paper74060.html
- Branford S, Seymour JF, Grigg A, et al. BCR-ABL messenger RNA levels continue to decline in patients with chronic phase chronic myeloid leukemia treated with imatinib for more than 5 years and approximately half of all first-line treated patients have stable undetectable BCR-ABL using strict sensitivity criteria. Clin Cancer Res 2007;13:7080-5. [Crossref] [PubMed]
- Hughes TP, Saglio G, Kantarjian HM, et al. Early molecular response predicts outcomes in patients with chronic myeloid leukemia in chronic phase treated with frontline nilotinib or imatinib. Blood 2014;123:1353-60. [Crossref] [PubMed]
- Jabbour E, Kantarjian HM, Saglio G, et al. Early response with dasatinib or imatinib in chronic myeloid leukemia: 3-year follow-up from a randomized phase 3 trial (DASISION). Blood 2014;123:494-500. [Crossref] [PubMed]
- Rea D, Nicolini FE, Tulliez M, et al. Dasatinib or nilotinib discontinuation in chronic phase (CP)-chronic myeloid leukemia (CML) patients (pts) with durably undetectable BCR-ABL transcripts: interim analysis of the STOP2G-TKI study with a minimum follow-up of 12months – on behalf of the French CML group Filmc. Available online: https://ash.confex.com/ash/2014/webprogram/Paper72021.html
- Tsutsumi Y, Ito S, Ohigashi H, et al. Unplanned discontinuation of tyrosine kinase inhibitors in chronic myeloid leukemia. Mol Clin Oncol 2016;4:89-92. [PubMed]
- Richter J, Söderlund S, Lübking A, et al. Musculoskeletal pain in patients with chronic myeloid leukemia after discontinuation of imatinib: a tyrosine kinase inhibitor withdrawal syndrome? J Clin Oncol 2014;32:2821-3. [Crossref] [PubMed]
- Ishii Y, Hagihara M, Kato A, et al. Musculoskeletal pain may be associated with imatinib withdrawal syndrome in chronic myeloid leukemia patients. Leuk Lymphoma 2015. [Epub ahead of print]. [PubMed]
- Breccia M, Efficace F, Sica S, et al. Adherence and future discontinuation of tyrosine kinase inhibitors in chronic phase chronic myeloid leukemia. A patient-based survey on 1133 patients. Leuk Res 2015;39:1055-9. [Crossref] [PubMed]
- Kijima M, Gardiol N, Held W. Natural killer cell mediated missing-self recognition can protect mice from primary chronic myeloid leukemia in vivo. PLoS One 2011;6:e27639. [Crossref] [PubMed]
- Kreutzman A, Rohon P, Faber E, et al. Chronic myeloid leukemia patients in prolonged remission following interferon-α monotherapy have distinct cytokine and oligoclonal lymphocyte profile. PLoS One 2011;6:e23022. [Crossref] [PubMed]
- Mizoguchi I, Yoshimoto T, Katagiri S, et al. Sustained upregulation of effector natural killer cells in chronic myeloid leukemia after discontinuation of imatinib. Cancer Sci 2013;104:1146-53. [Crossref] [PubMed]
- Kim DH, Kamel-Reid S, Chang H, et al. Natural killer or natural killer/T cell lineage large granular lymphocytosis associated with dasatinib therapy for Philadelphia chromosome positive leukemia. Haematologica 2009;94:135-9. [Crossref] [PubMed]
- Mustjoki S, Ekblom M, Arstila TP, et al. Clonal expansion of T/NK-cells during tyrosine kinase inhibitor dasatinib therapy. Leukemia 2009;23:1398-405. [Crossref] [PubMed]
- Legros L, Rousselot P, Giraudier S, et al. Second attempt to discontinue imatinib in CP-CML patients with a second sustained complete molecular response. Blood 2012;120:1959-60. [Crossref] [PubMed]
- Baccarani M, Deininger MW, Rosti G, et al. European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Blood 2013;122:872-84. [Crossref] [PubMed]
- Hughes TP, Ross DM. Moving treatment-free remission into mainstream clinical practice in CML. Blood 2016;128:17-23. [Crossref] [PubMed]
Cite this article as: Kimura S. Current status of ABL tyrosine kinase inhibitors stop studies for chronic myeloid leukemia. Stem Cell Investig 2016;3:36.


