
This article has an erratum available at: http://dx.doi.org/10.21037/sci-2021-01 the article has been update on 2021-08-12 at here.
Epidermal inclusion cyst in the thyroid gland
Introduction
Epidermal inclusion cysts (EIC) are common benign lesions of the skin, ovaries, and testicles. They develop from ectodermal tissue and contain squamous cells surrounded by a fibrous layer. Rarely are seen in mucosal or glandular tissue. They are only a few cases reported of epidermal cysts in thyroid tissue. In this report, we described a case of intrathyroidal epidermal cyst presented with dysphonia and dysphagia requiring surgical intervention.
We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/sci-2020-021).
Case presentation
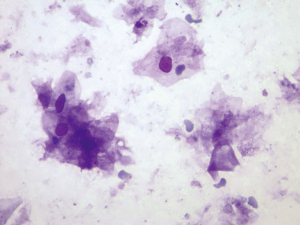
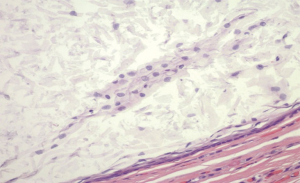
We present a case of a 57 years old male with a past medical history of nontoxic uninodular goiter, hypothyroidism referred from primary care for a thyroid nodule found on neck ultrasound. He endorsed dysphonia and dysphagia, clinically and biochemically euthyroid. The Thyroid ultrasound showed right thyroid lobe measures 4.9×2.0×3.2 cm3 and the left thyroid lobe measures 3.1×0.7×1.0 cm3. A right lobe nodule located at mid to lower pole, 3.1×1.8×3.2 cm3, cystic, hypoechoic with punctate echogenic foci, and smooth margins (Figure 1). Fine needle aspiration of the right thyroid lobe was performed and the cytology reported sheets of squamous in a background of necrotic and proteinaceous material, consistent with epidermal cyst (Figure 2). Patient underwent right lobectomy. Gross section demonstrated a cyst with solid and cystic area containing tan-brown cheesy materials. The surgical pathology exam confirmed the diagnosis of benign thyroid cyst, consistent with EIC of the thyroid (Figure 3).

All procedures performed in studies involving human participants were in accordance with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Discussion
EIC which is also known as epithelial or epidermoid cyst are common skin lesions; they represent approximately 85% to 90% of all excised cysts. However, the incidence of mucosal sites is rare, being 0.01% of all oral cavity cysts (1). They are benign, asymptomatic and slowly enlarging cysts (1,2). EIC are most commonly located on the trunk, neck, face, scrotum, behind the ears and in palmoplantar regions (1).
EIC in the thyroid gland is rare, and they are only 10 cases published as per Palombini et al. (3). Of those cases, 3 of them didn’t have fine needle cytology, and two were non-diagnostic (3). The etiology of EIC remains unknown and the most accepted theory is the reactivation of the remaining ectoderm trapped in the 1st and 2nd pharyngeal arches. However, the traumatic or surgical implantation of epidermal tissue into the thyroid gland may be associated with pathogenesis of EIC in thyroid (1-7). Typical sonography appearance are unilocular and well circumscribed, avascular hypoechoic to subcutaneous fat unless filled with thick mucoid, purulent, and/or hemorrhagic material. On cytology, they look as many mature superficial squamous cells with intact nuclei, anucleate squames, clusters of neutrophils and lymphocytes, macrophages, and in the background amorphous debris (4,5). Commonly they are unilocular and well-circumscribed, lined by squamous epithelium and surrounded by a fibrous layer with smooth muscle fibers. The risk of malignant transformation of EIC is rare. None has been reported in thyroid cases (4,6).
Squamous cells, the principal component of the epidermoid cysts, are not a component of the normal thyroid gland, but they may be seen in variety of thyroid lesions such as neoplasms, benign metaplasia, and congenital remnants. Tumors that contain them are papillary carcinoma, squamous carcinoma, mucoepidermoid carcinoma, adenosquamous carcinoma, and teratomas. Benign squamous metaplasia can happen in goiter, myxedema, and thyroiditis. It has been also seen in congenital remnants of thymus rests, thyroglossal duct remnant, and brachial cleft cyst (6).
EIC of the thyroid can present as a painless solitary nodule seen in the anterior part of the neck that moves with swallowing, and no associated lymph nodes. Dysphagia and dyspnea can occur if the cyst is large. The treatment of symptomatic EIC is surgical excision and the recurrence is unusual. There are no reported cases of recurrence in thyroid EIC (4).
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/sci-2020-021
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/sci-2020-021). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kuduban O. Epidermal inclusion cyst of thyroid gland. Eurasian J Med 2015;47:78. [Crossref] [PubMed]
- Yilmaz M, Haciyev Y, Mamanov M, et al. Epidermal inclusion cyst of the larynx. J Craniofac Surg 2011;22:e1-2. [Crossref] [PubMed]
- Palombini L, Cozzolino I, Luigi S, et al. Fine needle cytology of intrathyroid epidermoid cyst. Diagn Cytopathol 2015;43:390-1. [Crossref] [PubMed]
- Kulkarni SS, Vyas AS. Thyroid Epidermal Cyst – A Common Cyst, Rare Site. Natl J Med Res 2016;6:290-1.
- Chen KT. Fine-needle aspiration cytology of epidermoid cyst of the thyroid: report of a case and review of seven cases. Diagn Cytopathol 2007;35:123-4. [Crossref] [PubMed]
- Bekele W, Gerscovich EO, Naderi S, et al. Sonography of an epidermoid inclusion cyst of the thyroid gland. J Ultrasound Med 2012;31:128-9. [Crossref] [PubMed]
- Choure DD, Nichat PD, Agarwal S, et al. Epidermal cyst presenting as a solitary thyroid nodule: A Rare Case Report. J Med Sci Clin Res 2015;3:7139-42. [Crossref]
Cite this article as: Palacio MN, Gonzalez-Mosquera L, Rosenthal D, Kunar S, Tao Q, Gebre W, Liao H. Epidermal inclusion cyst in the thyroid gland. Stem Cell Investig 2020;7:18.


